Abstract
Introduction.The ubiquitous spreading of human herpes viruses (HHV) in nature, the variety of ways and methods of their transmission, ability of lifelong persistence in the host and pantropism lead to almost total infection of the adult population. In immunocompromised patients (pts) with blood system diseases HHV infections are characterized by severe complications and may cause death without proper diagnostics and treatment. HHV-6 is widely explored in pts after allogenic transplantation but its role in pts after chemotherapy (ChT) courses and autologous stem cell transplantation (ASCT) is not investigated enough.
Aims. To determine the rate of HHV-6 reactivation in pts with hematological diseases. To investigate the role of HHV-6 infection in pts with immunodeficiency after ChT and ASCT to define treatment tactics.
Methods. From January 2013 to July 2017 in hematology department of National Research Center retrospectively analyzed 273 pts with newly diagnosed hematology diseases (72-with acute lymphoblastic leukemia (ALL), 141 - acute myeloblastic leukemia (AML), 15-with high-grade B-cell lymphoma (BCL), 45 - aplastic anemia (AA). ALL was treated according to ALL 2009 protocol, AML - with standart «7+3» ChT, AA - with Antithymocyte Globulin or cyclosporine, BCLs - with R-EPOCH/R-HMA or R-EPOCH. We performed real time polymerase chain reaction (RT-PCR) for detecting HHV-6 DNA in cases of any clinical complication after ChT, in period of febrile neutropenia and post-transplant. The investigation included the samples of blood, cerebrospinal fluid, urine, feces, bone marrow, bronchoalveolar lavage (BAL), saliva, pulmonary effusion. Diagnostically significant criterion was the DNA detection of more than 500 copies/ml.
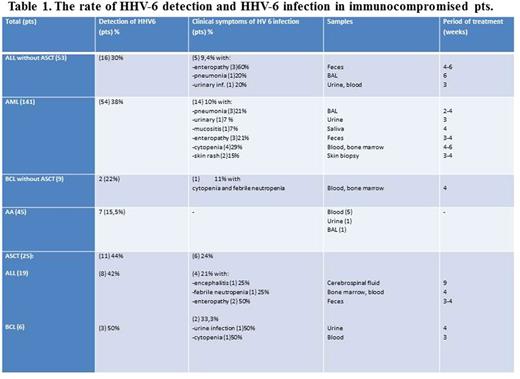
Results. HHV-6 reactivation was detected in 90 pts out of 273 (32,9%): 38% in AML pts (54 out of 141), 33% - in ALL pts (24 out of 72), in group of AA - 15,5% (7 out of 45), BCL - in 5 pts (33%). Twenty-five pts (19 with ALL, 6 - BCL) underwent ASCT. HHV-6 DNA was revealed in 44% cases of pts after ASCT, but only 24% of these pts received antiviral therapy because they had clinical symptoms of HHV-6 infection. The most severe infection was encephalitis. Among AML pts after ChT, manifestations of HHV-6 infections were detected in 14 out of 141 (10%), among ALL without ASCT- in 9,4% (5 out of 53). Before stating the HHV-6 infection and starting special treatment all other reasons of complications were excluded (bacterial and fungal). All pts with clinical symptoms of viral contagion received iv ganciclovir (10mg/kg/day) with further prophylaxis of valganciclovir (900mg/day) during 2-9 weeks. Almost all clinical symptoms regressed after 3-5 days of the treatment but DNA copies in samples stayed much longer (2-6 weeks) and early stop of treatment (1-2 weeks) in some cases caused the increasing of HHV-6 copies. Interestingly, that pts with AA didn't have clinical symptoms though had reactivation of HHV-6 and nobody of them needed antiviral treatment.
Conclusion. HHV-6 reactivation is quite common in immunocompromised pts (see table 1) but development of HHV- 6 infection requires treatment only in 9,5% (26 pts out of 273) of them (including pts after ASCT). The most severe complications associated with HHV-6 included encephalitis, enteropathy, urinary infection and pneumonia. More frequently HHV-6 was detected in blood samples and feces.The HHV-6 infection needs to be diagnosed when bacterial and fungal infections are excluded. In case without clinical symptoms there is no need to start specific treatment. When stated, HHV-6 infection requires continual antiviral curing until complete disappearing of DNA copies from biological liquids.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal